Neuromodulation is a last resort treatment for pediatric patients with epilepsy who haven't responded to medication and aren’t candidates for surgery. While these therapies can reduce seizures for some children with intractable epilepsy, they rarely eliminate their seizures all together. What's more, between 25% to 50% of children who receive neuromodulation therapies see little or no change in their seizure activity.
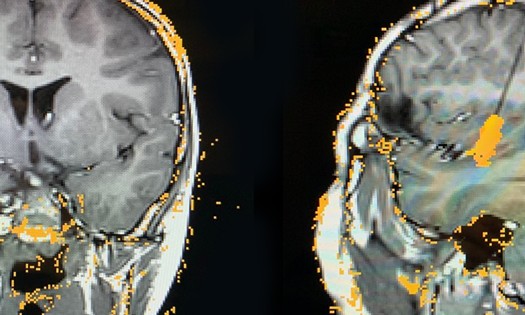
Neurologists and neurosurgeons at Children's Medical Center Dallas, part of Children's Health℠, are studying which areas of the thalamus are involved in a child’s seizure network. If a network includes the thalamus and can be disrupted, they may be able to reduce seizure activity for more children. During the diagnostic stage, they use invasive stereoelectroencephalography (SEEG) to pinpoint the thalamic nuclei involved in a child’s seizures. In the treatment phase, they are finding success with responsive neurostimulation (RNS) by placing the electrodes in areas of the brain most likely to disrupt seizure activity.
"Currently, not many pediatric programs monitor the thalamus prior to placing neuromodulation electrodes,” says Angela Price, M.D., Pediatric Neurosurgeon at Children’s Health and Associate Professor at UT Southwestern. "Gathering information with SEEG lets us make better decisions about which areas of the thalamus would benefit from neuromodulation so we can be more effective in helping kids who have no other treatment options”
Why it matters: Thalamic monitoring eliminates guesswork
It’s not always clear which areas of the brain are involved in seizures. But invasive SEEG monitoring of the thalamus can eliminate the guesswork. It provides information that helps neurosurgeons know which, if any, deep brain structures are involved in seizures and can be targeted during future therapies.
In their novel prospective study of 10 patients at Children’s Health, Dr. Price and her team are gathering data about thalamic SEEG to evaluate the benefits of thalamic monitoring for select patients who undergo SEEG, as well as the possible risks.
New modality: RNS provides more thalamic monitoring plus stimulation
RNS is the newest form of neuromodulation. Though currently FDA-approved for use in adults, physicians at Children’s Health have been using RNS with increasing frequency since 2021 on children as young as age 5. In pediatric epilepsy, physicians often use treatments that are off-label since studies are typically done in adults for medications and devices. Waiting for pediatric trials can delay good treatment options.
In 2023, 25 children received RNS at Children's Health, and the hospital is on pace to provide this modality to even more children in 2024. They’ve had success working with insurance companies to get RNS approved, giving the kids in their program more treatment choices.
RNS is a newer neuromodulation therapy and it is also unique in that it provides intracranial EEG data and stimulates the brain to disrupt seizures. The data helps neurologists program the stimulation to an individual child’s needs rather than relying on a preset program.
In adults, about 75% of patients have a 75% reduction in seizures two years after RNS implantation — a marked improvement on older neuromodulation therapies. Dr. Price and her team have seen the same or better results thus far with their pediatric patients.
Neurosurgery at Children’s Health: Leaders in epileptic care
For more than 20 years, the multidisciplinary team at Children’s Health has collaborated to provide the best care possible for children with epilepsy. Neurosurgeons, epileptologists, neuroradiologists and neuropsychologists work together and utilize advanced diagnostic tools – including 3D MRI, PET scan with glucose monitoring, SPECT studies, and neuropsychology testing – to develop highly personalized treatment plans for each patient.
Children’s Health is one of only a few pediatric centers in the country able to offer RNS and invasive EEG monitoring of the thalamus in children under age 18. Their center has the highest designation possible as a Level 4 Pediatric Epilepsy Center and offers advanced treatments, like robotic-assisted epilepsy surgeries, as well as clinical trials for new epilepsy medications. But Dr. Price says their team approach is what sets their program apart.
“We are fortunate to have a multidisciplinary group of colleagues who work together really well,” says Dr. Price. “Our team’s commitment to each other and to our patients is what allows us to provide such high-level care.”