By Nicolas Madsen, M.D., M.P.H., Co-Director of the Children’s Health℠ Heart Center and Chief of Cardiology at UT Southwestern
Just a few decades ago, many complex congenital heart conditions were fatal or, at best, palliated to enable a few years of survival. Thankfully, there’s been a great many medical advances and children with these conditions today have a less than 5% mortality rate nationwide. As we celebrate that these children go on to live longer lives than ever before, it presents extraordinary opportunities to make their medical management more precise to not only extend their life but greatly improve its quality.
At Children’s Medical Center Dallas, part of Children’s Health℠, we’re making progress in five key areas – harnessing the power of big data, innovating care for new and emerging patient types, addressing health inequities, preventing and treating neurodevelopmental conditions and pioneering minimally-invasive procedures. These efforts are all part of our mission to reshape the future of pediatric and congenital cardiology and help more children with heart conditions live long, healthy, fruitful lives.
Leveraging big data
There is an enormous amount of patient data available today – from electronic health record data and physiologic data collected at the bedside to genetics and population science data.
We recently hired Javier Lasa, M.D., a pediatric critical care cardiologist with expertise in applied informatics and data science, to develop novel ways to use precision medicine and transform care at our Heart Center. Dr. Lasa is building a technological infrastructure that includes cloud-based artificial intelligence and language processing tools, as well as a team of data scientists and analysts. We’ll use this infrastructure to uncover historical patterns in patient data that will help us better understand how to drive patient-specific improvement efforts.
Our ultimate goal is to combine multiple data sources in real-time at the bedside to better predict the testing and treatment that will achieve the best possible outcomes for each patient with the lowest risk of complications. We aim to empower our entire Heart Center team with these big-data tools to provide the most timely and effective care.
Innovating for new patient types
Patients with the most complex heart conditions are living far longer than we thought possible just a couple decades ago. That means we’re encountering new complexities in their lifelong care. Our Heart Center team is developing innovations to best treat these new patient types and significantly improve their quality of life.
For example, many of these patients face a higher risk of pulmonary hypertension. Megan Griffiths, M.D., recently joined our team and is bringing state-of-the-art treatment options to patients via our new Pulmonary Hypertension Program. This unique multidisciplinary program provides the full spectrum of current treatment options as well as opportunities to participate in clinical trials. The program’s goal is to not only continue to improve survival and decrease complications, but enable patients to have a greater quality of life.
Similarly, over the last decade, we’ve also developed a groundbreaking ventricular assist device (VAD) program directed by Ryan Butts, M.D., Pediatric Cardiologist, and Ryan Davies, M.D., Pediatric Cardiothoracic Surgeon. This program has enabled Children’s Health to develop a myriad of first-in-kind protocols that facilitate many gains, such as earlier discharge home. We recently safely discharged home a patient with a VAD only two weeks after receiving a device, which was unheard of a few years ago. Many of these protocols specifically target educating and supporting the family so they can safely care for their child at home.
Equalizing transplant care
Numerous studies have shown that health disparities driven by race, socioeconomic status and parents’ educational background can substantially impact health outcomes for many patients, including those who receive a heart transplant.
Mehreen Iqbal, M.D., recently joined our Pediatric Advanced Cardiac Care team and particularly focuses on the intersection of end-stage heart failure with diversity, equity and inclusion. Dr. Iqbal is leading our efforts to better understand how we can mitigate these differences to improve transplant outcomes. We’re studying important questions, such as:
How do outcomes vary for different VADs depending on a patient’s racial, socio-economic or family educational background?
What support and home health services do different patient subgroups need to optimize medication-related outcomes?
We’re also playing a leading role in the efforts to combine the Pediatric Acute Care Cardiology Collaborative data registry with the newly launched health equity module. This comprehensive acute care registry includes more than 70,000 hospitalizations. By integrating U.S. census data, we’ll gain important insights into modifiers of hospital length of stay, medications, complications and mortality.
Addressing neurodevelopmental impact
Pediatric cardiology patients have a higher risk of developmental delays and disorders such as attention deficit disorder. They’re also predisposed to mental health issues such as anxiety and depression.
Addressing these issues requires expertise that extends beyond cardiology. In 2011, we were one of the first heart centers in the nation to develop a multidisciplinary cardiac neurodevelopmental program bringing together expertise in clinical psychology, neurology and neonatology. Randi Cheatham-Johnson, Ph.D., is a clinical psychologist who recently joined our program to bring more therapies to our patients, including behavioral modification. We’re committed to continuing to expand our team, allowing for greater multidisciplinary and multi-center collaborations. We’re particularly focused on advancing care in three ways:
Developing standardized protocols to identify at-risk patients earlier
Researching therapies that could better protect the brain during vulnerable periods, including fetal life, during and immediately after birth and during and after surgery
Providing early and sustained access to treatment of developmental delays and mental health conditions
As we get better at identifying, preventing and treating these conditions, we’re collaborating and sharing our innovations with other centers, namely as part of the Cardiac Neurodevelopmental Outcomes Consortium.
Optimizing minimally invasive catheterization procedures
Plastic bronchitis is a lymphatic flow disorder that causes severe respiratory compromise. This condition can be a complication after Fontan surgery. Just a few years ago, the only available procedural treatment was invasive surgery. This treatment was often unsuccessful and involved a difficult recovery fraught with complications.
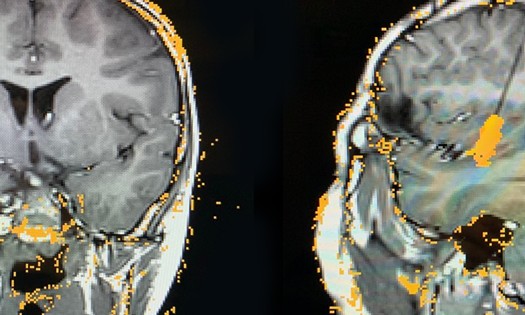
Tarique Hussein, M.D., our Director for Cardiac Magnetic Resonance Imaging, and Suren Reddy, M.D., our Director of Pediatric Interventional Cardiology, have pioneered a minimally invasive option to more successfully treat plastic bronchitis. This catheter procedure benefits from MRI guidance to pinpoint the location in the lymphatic circulation that requires intervention so we can occlude it with precision. It takes 10 to 12 hours to complete and requires enormous imaging and interventional expertise as well as a deep commitment to multidisciplinary collaboration.
This innovative approach is dramatically improving outcomes. Patients have a much easier recovery and are typically discharged home the next day.
By continuing to optimize this procedure, we’re redefining what’s possible for catheter approaches for this complex condition and others like it that impact our most vulnerable patients.
Learn more about innovative care at the Children’s Health Heart Center.>>