Hypotonia, ataxia and delayed development syndrome (HADDS) is a neurodevelopmental condition only recently defined and still largely unknown across the medical community. It is associated with symptoms like low muscle tone and developmental delay and is frequently accompanied by urinary abnormalities that physicians may misinterpret and treat unsuccessfully as a result.
Irina Stanasel, M.D., Pediatric Urologist and Assistant Professor at UT Southwestern who practices at Children’s Medical Center in Dallas, part of the Children’s HealthSM system, first encountered the nuances of treating HADDS through a patient she began seeing in 2017. The patient was undiagnosed at the time, but Dr. Stanasel led her through genetic testing and other steps that yielded life-changing answers and resolutions to her urinary dysfunction. “HADDS is unique, and providers must learn its idiosyncrasies to provide appropriate urological care and avoid complications such as urinary tract infections and renal scarring,” she says.
Recognizing diverse symptoms as part of one disorder
At 6 months old, the patient already had a history of urinary tract infections (UTIs) and vesicoureteral reflux (VUR). Imaging showed dilation of the urinary tract including a distended, thick-walled bladder and hydroureteronephrosis.
A physical exam and conversation with the mother revealed multiple other symptoms: low muscle tone, misaligned eyes (strabismus), and high pain threshold. Previous doctors had told the mother these findings were common in babies and unrelated to each other, but Dr. Stanasel suspected otherwise.
“As soon as I said, ‘Something is off, isn’t it?’ the mother was so grateful. She had been saying that for months, and no one listened,” she says.
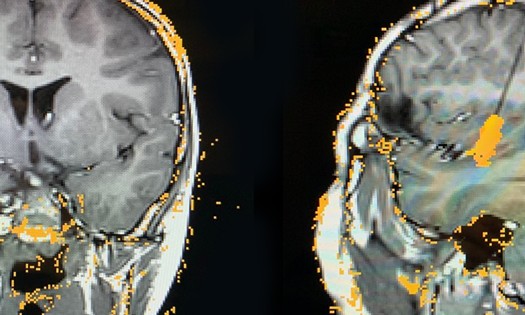
Dr. Stanasel started the child on a catheterization program, which promptly improved her hydronephrosis and the thickness of the bladder wall. Her UTIs and VUR resolved almost immediately as well. An MRI showed no lumbar abnormalities, which are common with spina bifida, but did reveal a subtle finding known as cerebellar vermis hypoplasia. This finding has since been associated with HADDS, but at the time the connection was unknown. In search of answers, Dr. Stanasel ordered a full genetic panel.
Getting a diagnosis – and a multidisciplinary team
Genetic testing revealed a mutation in the EBF3 gene – which had just recently been linked to HADDS.
“Finally, the family had the answer they were searching for, and I knew what other care the child required,” says Dr. Stanasel.
In addition to Dr. Stanasel, a urologist, the patient is now seen by a neurologist, occupational therapist, gastroenterologist and ophthalmologist. They have provided various treatments over the years, including botulinum toxin injections to reduce muscle spasticity in the legs and multiple interventions to aid with stooling.
While neurologists tend to lead care for HADDS patients, Dr. Stanasel says urologists play a critical role. “The urinary complications are the ones that can make children with HADDS the sickest – kidney infections and renal scarring. So, this part of their care often needs the most urgent and informed attention,” she explains.
VUR caused by a tight urethral sphincter
The urological presentation of HADDS is easy to misread. It may include urinary incontinence, an intermittent urine stream, urinary tract infections or abnormal renal ultrasound results. Children may be found to have vesicoureteral reflux on a voiding cystourethrogram.
One mistake is to assume spina bifida.“Spina bifida is typically associated with a small bladder with poor compliance, while HADDS patients typically have a distended bladder and urinary retention,” explains Dr. Stanasel.
Another mistake is to treat their reflux with antibiotics or surgery. With HADDS, reflux is caused by an inability to relax the urethral sphincter during the voiding phase, which leads to urine lingering in the bladder and backing up to the kidneys. “These children don’t need ureteral reimplantation, they need to empty their bladders,” says Dr. Stanasel.
After a few years on an intermittent bladder catheterization program, the patient became resistant to being catheterized and required a vesicostomy – a procedure that enables urine to drain from the bladder directly outside the body through a tiny stoma in the lower abdomen. The patient has been UTI free since her surgery, and renal imaging has shown normal kidneys without dilation.
Why Children’s Health Urology: Building a knowledge base around HADDS
Dr. Stanasel now sees multiple patients with HADDS and has published a paper on the urinary abnormalities that often accompany it. She says an early and accurate diagnosis is important to provide the necessary urinary interventions and give patients maximum support for their developmental needs.
Symptoms to watch for
Low muscle tone (hypotonia)
Poor muscle control (ataxia)
High pain threshold
Delays in motor skills, speech and/or cognition
Strabismus or other facial abnormalities
Recurrent UTIs, VUR or other urinary problems
Unique urological aspects
Renal ultrasounds may be normal or abnormal
Recurrent UTIs
Intermittent urinary stream
Detruso-sphincter-dyssynergia
Possible abnormalities of the genitalia
Putting families at ease
Led by the EBF3 HADDS Foundation, a community of families, providers and advocates is rapidly forming to support each other and spread awareness of the disease. Dr. Stanasel cites this as another pivotal benefit of getting the right diagnosis. “Families can spend years feeling adrift without answers. Once they know it’s HADDS, they have a community to anchor them,” she says.
Learn more about innovative urology care at Children’s Health >>