The American Academy of Otolaryngology–Head and Neck Surgery Foundation significantly revised the pain management recommendations related to tonsillectomy, and made other key guideline recommendations to help reduce complications and enable faster recoveries.
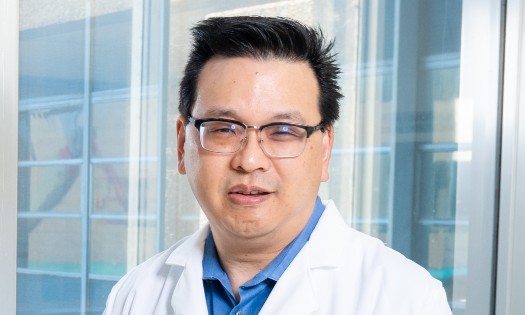
“The 2019 guideline update aims to improve pain management, and outline key changes like recommending tonsillectomy for children with obstructive sleep apnea,” says Ron Mitchell, M.D., Division Director of Ear, Nose and Throat at Children’s Health℠ and Professor at UT Southwestern. Dr. Mitchell chaired the guideline update group.
The guideline has changed in four key areas:
1. Pain Management: Ibuprofen/Acetaminophen Vs. Codeine
The updated guideline recommends prescribing ibuprofen and/or acetaminophen instead of codeine and other opiates.
Some physicians and parents have been hesitant to use ibuprofen because of concerns that it increases postoperative bleeding. But a review of multiple studies found that ibuprofen and acetaminophen effectively control pain and do not increase bleeding risk or the number of bleeding events requiring surgical intervention.
This is in line with the FDA’s black box codeine warning due to the risks of overdose and death in children who are ultra-rapid codeine metabolizers. The American Academy of Pediatrics has also recommended against the use of codeine in children under 18.
2. New Emphasis on Pain Counseling
The updated guideline recommends counseling caregivers about the importance of pain assessment management – before and after tonsillectomy.
“Pain after tonsillectomy can lead to dehydration, and dehydration can lead to bleeding,” says Dr. Mitchell, whose team performs around 2,500 tonsillectomy procedures a year.
The updated guideline calls for providing preoperative verbal and written information about pain, how to manage it, and what pain medication with dosage to use. The guideline also recommends reinforcing that information after tonsillectomy.
“It’s really important to include the children and caregivers in these conversations – especially adolescents,” Dr. Mitchell says. “A parent can’t really hold an adolescent down and give them pain meds. Having these conversations helps get their buy-in so they’re more likely to take pain medication and fluids and recover faster and without complications.”
3. More Evidence Against Routine Perioperative Antibiotics
The previous, 2011 tonsillectomy guideline recommended against prescribing routine antibiotics – and the evidence has become even stronger since then. The new guideline cites a Cochrane review of 10 trials that showed antibiotics do not reduce pain, bleeding or the need for pain medication.
“There are certain situations that still warrant antibiotics, like a child with heart disease who may face anesthesia complications,” Dr. Mitchell says. “But there’s no evidence to support routine use of antibiotics. That explains why the percentage of otolaryngologists who routinely use antibiotics after tonsillectomy has dropped from 80 to 90 percent, to less than 20 percent.”
4. Watchful Waiting for Recurrent Throat Infections
Like the 2011 guideline, the 2019 update emphasizes “watchful waiting” for recurrent throat infections that are not frequent or severe. This recommendation has been changed to a strong recommendation.
The guideline recommends watchful waiting if a child does not meet the Paradise criteria: less than seven infections within the year, less than five per year in the past two years, or less than three per year in the past three years.
“Increasingly, the evidence shows that children who don't reach this criteria have a tendency to improve without tonsillectomy within 12 months,” Dr. Mitchell says.
Tonsillectomy Helps Kids with Obstructive Sleep Apnea
Another key change: the updated guideline recommends tonsillectomy for children with obstructive sleep apnea confirmed by sleep study. This reflects evidence from recent studies like the Childhood Adenotonsillectomy Trial (CHAT), which found that tonsillectomy improved obstructive sleep apnea symptoms, behavioral outcomes and quality of life.
“After tonsillectomy, many kids in the study slept better, which led to positive benefits like improved attention span,” Dr. Mitchell says. “We recommend tonsillectomy for children with obstructive sleep apnea who have had issues for over three months that have not improved or gotten worse.”
Full Guideline and Resources Available Online
Dr. Mitchell and his team often field questions from primary care physicians, otolaryngologists, patients and families about when to perform tonsillectomy. That's one reason he and his colleagues created easy-to-use reference guides and handouts, for patients and families. These are available at ENTnet.org.
“It’s not easy to stay up-to-date on all the different recommendations, especially for primary care providers who juggle so many patients,” Dr. Mitchell says. “We hope these resources are helpful to them, and my team is always happy to answer questions about particular cases.”
To learn more about tonsillectomy or to refer a patient, please call [214-456-9933](tel: 214-456-9933) or visit childrens.com/ENT.