When medications failed to manage a teenage patient's inflammatory bowel disease (IBD), the gastroenterology and surgery teams at Children’s Medical Center Dallas, part of Children’s Health℠, collaborated through a new multidisciplinary clinic – one of the first of its kind in the nation.
The patient has Crohn’s disease affecting the terminal ileum, which characterizes 20% to 30% of pediatric Crohn’s disease patients. This subset of Crohn’s disease progresses rapidly, and like many patients with this condition, he had developed a partial intestinal obstruction. His quality of life and overall health were greatly impacted by his ongoing symptoms despite optimized medical therapy. Malnourished and underweight, he lacked an appetite and experienced abdominal pain when eating. Generally, very athletic, the patient was limiting his physical activity because of his symptoms.
Children’s Health launched its new clinic in November 2022 to provide the best patient experience and outcomes for IBD patients that benefit from surgery, like this teenager. The clinic integrates GI and surgery so these two specialties see and treat IBD patients together. The clinic’s GI lead is Bhaskar Gurram, M.D., Director of the UT Southwestern Pediatric IBD Program at Children’s Health and Associate Professor at UT Southwestern, and the surgery lead is Samir Pandya, M.D., Pediatric Surgeon at Children’s Health and Associate Professor at UT Southwestern.
“Together, we met with the patient and his family from the first conversation about the surgical treatment plan,” Dr. Pandya says. “We were able to help ease their fears by explaining the minimally invasive techniques and protocols we planned for each point in this patient’s journey – all of which contributed to only a three-day hospital stay after surgery, and ultimately IBD remission.”
The benefit of patient-facing collaboration
At many pediatric centers an IBD surgical patient doesn’t meet the surgeon until closer to surgery, or they may need separate appointments to meet with the gastroenterologist and surgeon. By working together with the patient from the beginning of the surgical treatment plan, the clinic provides a better, more streamlined patient experience. Patients learn about the medication and surgical aspects of the treatment plan at the same time, and they get their questions answered from both experts.
This family’s questions and concerns were related to the risk of an ostomy, the size of the incision, the length of the recovery, the amount of pain the patient might experience, and how long he'd stay in the hospital. The family also had questions about his care after recovering from the procedure, including the medications he would need to continue.
“The patient also wanted to know when he could get back to playing sports. Since we plan for recovery ahead of this first meeting, this conversation is an opportunity for us to set expectations for these kinds of concerns. We explained how we keep risks to an absolute minimum, so patients have the easiest and fastest recovery possible. This upfront education helped them feel as comfortable as they can about the entire process,” Dr. Pandya says.
The team educated the family on processes like total parenteral nutrition (TPN) before surgery, the laparoscopic procedure with minimal incisions and an enhanced recovery protocol. These techniques and protocols contribute to nation-leading outcomes for pediatric IBD surgeries at Children’s Health, such as an average hospital stay of 4 to 4.5 days and a less than 5% infection rate.
Preoperative care improves recovery, prevents infection, and manages pain
Because this patient was malnourished, he received TPN for about a week before surgery to strengthen his body and improve his chances of a fast recovery.
“The high protein content from TPN helps the body switch from a catabolic state to an anabolic state,” Dr. Pandya says. “This protocol is really beneficial for malnourished patients to help minimize the risk of breakdown of the anastomosis or the wound after surgery.”
The team also has standard preoperative protocols to minimize the risk of infection. Patients shower at the hospital and chlorhexidine wipes are used to sanitize the surgical area. Patients also receive IV antibiotics, which are completed before surgery begins.
“We aim to have the antibiotics administered into the patient prior to making the incision. This practice is thought to decrease the risk of infections related to surgery,” Dr. Pandya says.
To preemptively treat pain, the team administers non-opioid pain medication prior to surgery. This protocol is shown to reduce the need for opioid medication during recovery.
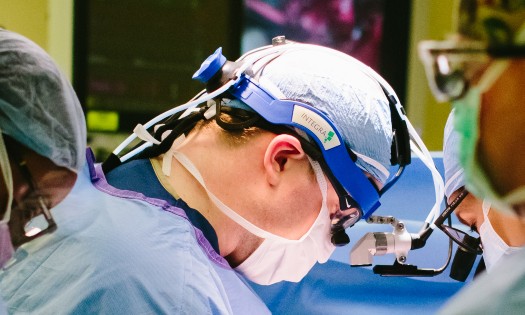
Laparoscopic ileocolectomy through one incision
Children’s Medical Center Dallas is a Level I Children’s Surgery Center designated by the American College of Surgeons, which recognizes its deep commitment to surgical excellence and innovation. The surgeons who practice here perform the most pediatric minimally invasive procedures in the region. The team approaches these procedures to minimize incisions and make them as cosmetically appealing as possible, while ensuring safety and quality.
For this patient, Dr. Pandya made one 4-inch Pfannenstiel incision for the laparoscopic ileocolectomy. The team performed the laparoscopic mobilization and evaluation of the bowel through this single incision using a specialized port.
“You need an incision of about this size to extract the specimen, but instead of creating this incision and others for the camera and laparoscope, we just used one to perform the procedure,” Dr. Pandya says. "That way, the patient only has one scar discreetly placed below the underwear line and less scar tissue."
Discharged after three days, and now in remission
The team moved the patient to recovery and began the enhanced recovery protocol, including a clear liquid diet as soon as he was awake, early ambulation and non-opioid pain medication.
“The goal of these protocols is to get the intestines functioning as soon as possible after surgery so patients have a faster, easier recovery and a shorter hospital stay,” Dr. Pandya explains.
The patient was discharged three days after the surgery. He had an uneventful recovery and was able to resume sports within six weeks.
He’s continued his IBD medication to manage the disease, and as of January 2023, his IBD is now in remission. He has improved energy, appetite and physical activity.
This case study illustrates Children's Health’s commitment to innovation and multidisciplinary collaboration as a national leader in IBD outcomes and remission rates.