When a child experiences abdominal pain and vomiting, it’s reasonable to assume the cause is constipation or a digestive issue. But when the episodes repeat over time, it might signal a potentially more serious condition that can go undiagnosed: ureteropelvic junction obstruction (UPJO) presenting as Dietl’s crisis.
The urology team at Children’s Health℠, home to Children’s Medical Center Dallas, has seen patients with UPJOs that weren’t recognized for months or even years. This can delay treatment and subject children to unnecessary procedures, as physicians investigate other potential causes of pain and emesis. That’s why Micah Jacobs, M.D., Pediatric Urologist at Children’s Health and Associate Professor at UT Southwestern, is eager to share tips and insights from our experience.
“Many physicians aren’t familiar with Dietl’s crisis, but diagnosing a UPJO and correcting it via pyeloplasty is fairly straightforward once you know to look for it,” says Dr. Jacobs.
Ureteropelvic Junction Obstruction Symptoms
The majority of UPJOs are caused by a congenitally narrow ureter. Less commonly, a blood vessel can cause a constriction by crossing the ureter at the UPJ.
Presentation via Dietl’s crisis is similar to a kidney stone: acute (and sometimes severe) abdominal pain, often accompanied by nausea and vomiting. The pain is triggered by hydronephrosis, which occurs when a urine buildup can’t easily drain via the constricted UPJ. These episodes can be brought on by high fluid intake and/or consumption of a diuretic such as caffeinated soda.
“Patients don’t typically report urological issues associated with these episodes, so it makes sense that physicians don’t think of the kidneys as part of their evaluation — we recently saw a patient who had been thought to have a cyclic vomiting syndrome,” Dr. Jacobs says.
Investigating Via Ultrasound: Timing is Key
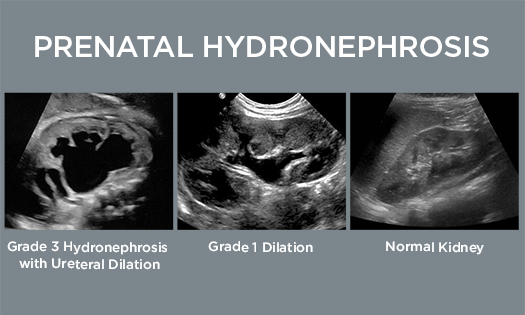
UPJOs are relatively easy to identify via ultrasound but in certain, more subtle cases the timing has to be right because the kidney needs to contain enough urine to trigger hydronephrosis.
“When we suspect a UPJO but it’s not detected via ultrasound, we’ll often recommend a patient waits until the next time they’re in pain, and then goes to the emergency department for an ultrasound,” Dr. Jacobs says. “That significantly increases the likelihood of seeing the UPJO.”
When to Order a MAG-3 Study for Ureteropelvic Junction Obstruction
MAG-3 renograms use radiolabeled medication to assess kidney structure and function, and to identify blockages. These studies can be useful if a physician suspects a UPJO but an ultrasound is inconclusive, or if a child is experiencing significant pain even though the blockage appears relatively minor.
“An ultrasound is usually sufficient, but MAG-3 studies are a very effective way to make a definitive diagnosis when some questions remain,” Dr. Jacobs says.
The Children’s Health team counsels patients to pay close attention to their pain levels during the MAG-3 study. Lasix is administered as part of the study, causing the kidney to produce elevated amounts of urine. If a patient’s pain increases after they receive the Lasix, it helps confirm the pain is caused by a UPJO.
MAG-3 studies also help Dr. Jacobs and his colleagues gain a complete picture of kidney function.
“A kidney can lose function if it has been blocked for a very long time, and we may need to consider removal if it isn’t functioning well,” Dr. Jacobs says.
Robotic-Assisted Pyeloplasty for UPJO
Pyeloplasty can be curative for UPJOs. Once an obstruction is identified, Dr. Jacobs and his colleagues educate families about their options.
The Children’s Health team generally avoids pyeloplasties for newborns and often follows these younger patients for months or years without surgery, as some of these obstructions will resolve on their own. Some extenuating circumstances such, as a previous infection in the affected kidney, prompt earlier intervention.
When surgery is appropriate, Dr. Jacobs and his colleagues advise families about the differences between open and robotic surgery.
“Some families prefer open surgery and we’re happy to accommodate that, but most families opt for robotic surgery,” Dr. Jacobs says.
All of the urologic surgeons practicing at Children’s Health are certified in the Da Vinci Surgical System, which enables the team to perform pyeloplasty via 8mm incisions. The team uses the HIDES technique.
“That keeps the incisions below the bikini line and ensures that scars are not generally visible, which helps children avoid feeling self-conscious in the future,” Dr. Jacobs says.
The Children’s Health Difference
Children’s Health has some of the nation’s highest pediatric robotic surgery volumes, with pyeloplasties comprising approximately 90% of those surgeries. Led by Craig Peters, M.D., Division Director of Pediatric Urology at Children’s Health and Professor at UT Southwestern, the urology team’s expertise extends to many other procedures, including robotic heminephrectomy ureteral reimplantation, and uretero-ureterostomy. Our outcomes are consistent with other top centers nationwide.
“We take a collaborative approach that includes group discussions about how to approach complex cases,” Dr. Jacobs says. “That enables us to capitalize on the decades of shared expertise within our department, so we can find the best solution for each patient.”
Learn more about the innovative discoveries happening in the Children’s Health urology department.